ICD Codes: The Language of Healthcare Data and the Road Ahead with ICD-11
International Classification of Diseases (ICD) is essentially the universal language of healthcare data that drives everything from insurance reimbursements and risk adjustment models to public health reporting, clinical research, and quality tracking.
And now, with ICD-11 on the horizon, the healthcare industry is gearing up for the next big leap forward. But to understand what’s coming, we first need to look back at how far we’ve come from ICD-9 to ICD-10, and the growing pains that came with that transition.
ICD-9: The Limitations of a Bygone Era
ICD-9, developed in the late 1970s, was relatively simple by today’s standards. It included around 13,000 diagnosis codes, using 3 to 5 alphanumeric characters.
At the time, it did the job. But medicine has changed drastically in the last few decades. New diseases have emerged, diagnostic technology has evolved, and value-based care has become the norm. ICD-9 just couldn’t keep up. It lacked the flexibility, space, and specificity to support modern healthcare demands.
ICD-9 ran out of room, both structurally and clinically.
ICD-10: A Giant Leap in Clinical Precision
ICD-10 came with about 68,000 diagnosis codes and introduced 3 to 7-character alphanumeric codes for far greater granularity. It was developed by the World Health Organization (WHO) in the 1990s and widely adopted globally throughout the early 2000s.
Despite its availability, the U.S. delayed full adoption until October 1, 2015, when ICD-10-CM (for diagnoses) and ICD-10-PCS (for procedures) finally replaced ICD-9 across the American healthcare system. While countries like Canada, Australia, Germany, and France had already made the switch years earlier, the U.S. transition was slow, expensive, and complex.
The Rough Road from ICD-9 to ICD-10: Key Challenges
The benefits didn’t come easy. Here’s what the U.S. faced during the ICD-10 transition:
- Massive Costs: Updating systems, retraining staff, and modifying workflows cost the U.S. healthcare system an estimated $5–10 billion.
- Payment Delays & Denials: New code structures led to confusion, denied claims, and AR delays, especially for smaller clinics.
- Drop in Productivity: More detailed codes required longer documentation times, reducing the number of claims processed daily.
- Training Gaps: Coding professionals needed deep knowledge of anatomy and medical terminology. Skilled coders were in short supply.
- Complex Mapping: Few codes had one-to-one matches between ICD-9 and ICD-10, especially in specialties like OB/GYN, ER, and oncology.
- Impact on Research: Inconsistent mappings and coding errors affected the reliability of population health data, analytics, and quality metrics.
Why ICD-10 was worth the pain
Despite the massive costs and workflow disruptions, ICD-10 brought major benefits:
- Greater Specificity = Better Data: Providers could document complications, comorbidities, and outcomes in far more detail, improving billing accuracy and clinical tracking.
- Alignment with Global Systems: ICD-10 enabled better international comparisons, essential for research and public health responses (like pandemics).
- Support for Value-Based Care: Risk adjustment and quality reporting became more precise—critical for alternative payment models.
- Operational Efficiency: Though tough at first, ICD-10 improved EHR integration, claims processing, and data analytics.
So yes, the transition was painful—but necessary. And in the long run, it laid the foundation for more accurate healthcare data, better reimbursement practices, and stronger clinical research.
ICD-11: Built for the digital age
ICD-11, officially released by the WHO in 2018, came into effect globally on January 1, 2022, is a complete digital-first redesign developed for integration into modern EHRs, apps, and health data platforms. Here’s what makes ICD-11 different,
- Massive scope: The foundation component, a multidimensional collection of entities that can have multiple parents and child nodes with tens and thousands of concepts.
- Digital native: Built with an API-first approach, ICD-11 is designed for automated coding, AI support, and real-time analytics.
- Polyhierarchical structure: Diagnoses can be classified through multiple pathways, offering more flexibility.
- SMART coding: Combines stem codes with extension codes to capture severity, cause, location, and more—all in one cluster.
- New chapters: Includes entirely new sections like Traditional Medicine, Sexual Health, and Gaming Disorder—reflecting today’s health priorities.
- Built-in guidance: Clinical definitions and guidelines are embedded to reduce coding ambiguity.
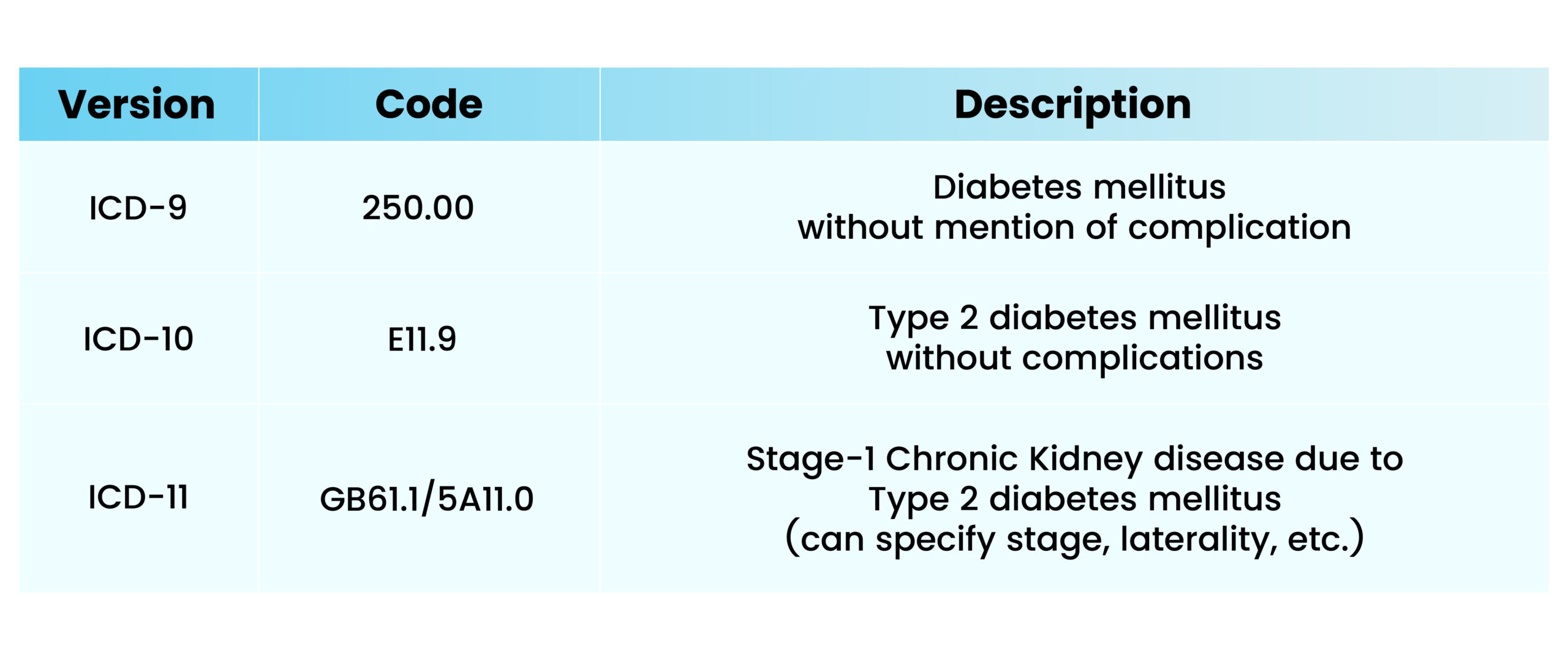
Example of Evolution
So, what’s the holdup in the U.S.?
While WHO reported that 64 countries were in various stages of implementation by February 2023, the U.S. is still on ICD-10-CM and ICD-10-PCS. The U.S. doesn’t use base ICD. Instead, ICD-10-CM (diagnoses) and ICD-10-PCS (procedures) are U.S.-specific versions managed by CDC/NCHS (Center for Disease Control & Prevention/ National Center for Health Statistics) and CMS (Centers for Medicare & Medicaid Services). As of now, there’s no mandated timeline for U.S. adoption of ICD-11. Here’s why:
- Creating ICD-11-CM/PCS would be a massive undertaking, requiring years of development, testing, and system updates.
- High cost of transition
- Extensive training required
- Data privacy and security concerns with a fully digital, integrated system
- Rebuilding legacy systems and payer infrastructures
From administrative codes to intelligent healthcare data
The evolution from ICD-9 to ICD-10—and now to ICD-11—is more than just a code upgrade. It marks the transformation of health information from an administrative burden to a powerful tool for clinical precision, data-driven care, and global collaboration.
ICD-11 is the future of diagnosis coding. Countries like Germany, the UK, China, Japan, Saudi Arabia, Korea, and Brazil are already making significant strides in clinical adoption.
The long-term benefits of ICD-11—improved patient outcomes, more efficient healthcare systems, and a powerful new tool for medical discovery—make its global adoption an inevitable and critical step forward for 21st-century healthcare. It marks the evolution of health information from a simple administrative tool to a dynamic, intelligent resource at the heart of medical progress.

